The way we treat chronic illnesses is being revolutionized by automated medication management systems, or AMMS. The ultimate goals of these intelligent systems are to improve patient adherence, expedite drug scheduling, and improve healthcare outcomes.
With AMMS, patients may benefit from increased sense of control over their health, decreased prescription errors, and better drug adherence. Improved patient communication, less medication-related problems, and enhanced efficiency are all advantageous to healthcare professionals. In terms of society, AMMS can save healthcare costs by reducing readmissions to hospitals and enhancing general health.
However, there are several engineering difficulties in creating a solid and trustworthy AMMS. Now let’s examine the main problems and possible fixes.
Medication Adherence
The act of taking prescription drugs as directed, or medication adherence, is still a major challenge. Many patients do not take their medications as directed by the clinicians, which can have detrimental repercussions on their health. There are several technological ways to increase adherence:
- Reminders for medications: To make sure patients don’t forget doses, automated systems and mobile apps can send out timely, customized reminders. Machine learning algorithms that examine patient behavior and preferences can be used to customize these reminders.
- Automated pill dispensers: These devices can automatically deliver pre-sorted pills at predetermined intervals while offering visual cues and reminders. When these systems are integrated with Internet of Things (IoT) devices, they can offer real-time feedback and adjustments.
- Real-time monitoring: Sensor-equipped smart pill bottles can recognize when they are opened and track the amount of medication taken. Wearable sensors are able to track physiological indicators that show whether or not a medication has been taken. If a dose is missed, this information can be forwarded to medical professionals for prompt action.
Interoperability and Data Integration
Data from a variety of sources, such as wearables, drug dispensers, and Electronic Health Records (EHRs), is used by automated medication management systems, or AMMS. However, a lack of uniformity frequently results in fragmented data in healthcare systems. Because of this, it is difficult to seamlessly combine data and present a complete picture of a patient’s medication schedule.
Here are some possible fixes:
- Fast Healthcare Interoperability Resources (FHIR): Developing a standard that offers a single language for electronic health data exchange.
- Standardization initiatives: To provide uniform data formats and exchange protocols, industry-wide projects like the Integrating the Healthcare Enterprise (IHE) initiative are essential.
- API Integration: Creating reliable APIs that facilitate safe and easy data transfer between various medical systems and equipment.
- Privacy and Security: Ensuring confidentiality protects patient trust, complies with laws like HIPAA, maintains data integrity, and guards against cybersecurity threats. AMMS should implement encryption, access controls, regular security audits, staff training, and incident response plans to safeguard this information effectively.
Here’s how to deal with these issues:
- Encryption: Unauthorized access and data breaches can be avoided by implementing robust encryption mechanisms (such as AES-256) for data that is in transit and at rest.
- Access control: By putting Role-based Access Control (RBAC) and Multi-factor Authentication (MFA) into place, you can make sure that only individuals with the proper authorization may access patient data.
- Compliance with regulations: AMMS must follow data privacy requirements including HIPAA and GDPR.
Technologies and Engineering Solutions
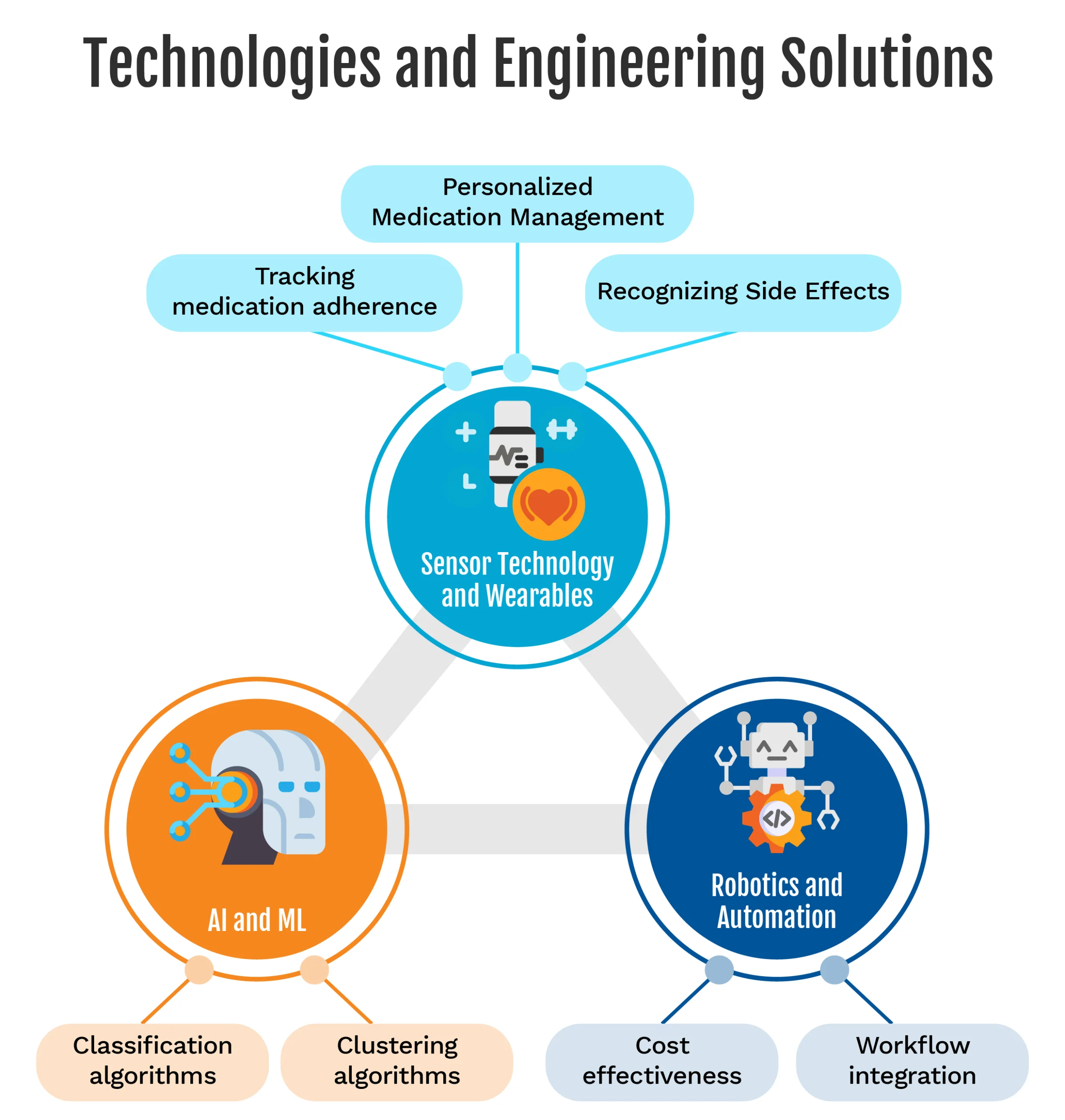
AI and ML:
Large volumes of patient data can be analyzed by machine learning algorithms, which can then be used to forecast adherence problems, identify possible adverse effects, and customize prescription schedules. Several pertinent algorithms consist of:
- Classification algorithms: Based on past data, patient behavior, and environmental factors, logistic regression, decision trees, and Support Vector Machines (SVMs) can forecast the probability that a patient would miss a dose.
- Clustering algorithms: Specific interventions can be implemented by identifying patient groups with comparable drug regimens and adherence habits using algorithms such as k-means and hierarchical clustering.
Sensor Technology and Wearables:
Vital signs, medicine ingestion habits, and even the body’s reactions to drugs can all be monitored via wearable sensors. You can use this info for:
- Tracking medication adherence: Activity trackers and smartwatches with accelerometers and gyroscopes can identify patterns of movement linked to taking medicine, like raising a glass of water or shaking a pill bottle.
- Recognizing side effects: Early intervention is made possible by the ability of sensors to monitor vital signs such as blood pressure, glucose levels, heart rate, and other parameters to identify possible medication side effects.
- Personalized medication management: By integrating wearable data with AMMS, medication schedules can be customized to a patient’s needs and lifestyle, maximizing adherence and reducing side effects.
Robotics and Automation:
Medication dispensing and pill sorting can be automated by robotic devices, increasing productivity and accuracy in medical environments. Still, there are obstacles to overcome:
- Cost-effectiveness: Putting robotic systems into place can be costly. Cost-justification must be achieved through increased effectiveness, decreased mistakes, and better patient outcomes.
- Workflow integration: Robotic systems need to be created with ease of integration into current hospital and pharmacy workflows. Custom software development and process redesign may be necessary to guarantee seamless operation and adoption.
A leading inventory management software provider wanted to build a safe inventory management system to track high-end medical SKUs for their international market. The task at hand was developing the system, releasing it ahead of schedule, and gaining a competitive advantage in the market. eInfochips helped the customer create a tracking software that can be integrated with RFID scanners for inventory monitoring and with biometric access and identity management systems for user mapping. To comply with HIPAA, the setup also needed to be integrated with the purchasing, billing, and patient information systems. Read more about the success story.
The Road Ahead
The AMMS has a promising future. Data collection and analysis can be further enhanced by emerging technologies such as the IoT, which can seamlessly connect devices and sensors. AI-driven DSSs can help medical professionals make wise choices about medication administration. In the end, AMMS offers a patient-centric approach to medication management that has the potential to completely transform the healthcare industry. As long as engineering and technology continue to progress, these systems will get more complex, which will benefit patients’ quality of life and results. Ensuring user-friendliness, scalability, and interoperability will be essential for success and widespread adoption.